TMJ Occlusion
The jaw joint is also known as the 'temporomandibular joint', known for short as the 'TMJ'. The makeup of the temporomandibular joint includes the hinge jaw joint (the bridge for the lower jaw or mandible) and temporal bone of the skull located in front of each ear, the muscles surrounding the jaw, and the jaw itself. It can be felt by placing your fingers just in front of your ears, and opening and closing your mouth
- TMJ (TEMPOROMANDIBULAR JOINT)
- Bruxism
JAW JOINT (TEMPOROMANDIBULAR JOINT) DISORDER
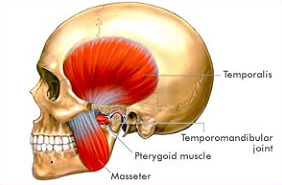 The jaw joint is also known as the 'temporomandibular joint', known for short as the 'TMJ'. The makeup of the temporomandibular joint includes the hinge jaw joint (the bridge for the lower jaw or mandible) and temporal bone of the skull located in front of each ear, the muscles surrounding the jaw, and the jaw itself. It can be felt by placing your fingers just in front of your ears, and opening and closing your mouth.
The jaw joint is also known as the 'temporomandibular joint', known for short as the 'TMJ'. The makeup of the temporomandibular joint includes the hinge jaw joint (the bridge for the lower jaw or mandible) and temporal bone of the skull located in front of each ear, the muscles surrounding the jaw, and the jaw itself. It can be felt by placing your fingers just in front of your ears, and opening and closing your mouth. The joint allows the jaw to open, close and move to the side and forward. It plays an important role in jaw functions such as talking, chewing, bite (occlusion) and yawning. It is one of the most complex and frequently used joints in the body. A TMJ disorder may affect one or both joints, often causing pain and limiting jaw function. Symptoms usually arise in early adulthood, but children and the elderly can also be affected.
Symptoms of TMJ include:
- Chronic headaches or migraines
- Discomfort when chewing or biting
- Grating, popping, or clicking sound when moving the jaw
- Aching facial pain
- Tenderness in the jaw
- Earache
- Limited range of motion or locked jaw
Diagnosis of TMJ Disorders
- An accurate diagnosis is very important to ensure that the right treatment is undertaken. Before starting treatment your dentist will make a diagnosis based on a clinical examination and your medical and dental history. During the examination the dentist will note the exact location of pain, stiffness or soreness, the range of jaw movement and any noises in the jaw joint. The dentist may examine your bite, tooth wear and movement of teeth. To assist with diagnosis your dentist may recommend.
- Plaster moulds of your teeth to see if your occlusion (bite) is correctly balanced.
- An X-ray examination.
- Completion of a questionnaire and a pain diagram to assess how your symptoms affect your quality of life.
- While there are certain medical conditions, such as arthritis, that may be involved in the development of TMJ disorder, the most common cause that we see is bruxism.
WHAT IS BRUXISM ?
Bruxism is an excessive clenching or grinding of the teeth that is not a part of normal chewing movements. It can lead to excessive wear on the teeth and may cause permanent damage to the teeth and the jaw joints. Excessive clenching and grinding are not normal, healthy actions of the jaws. In some adults and children, clenching and grinding may occur during the day or at night. They typically have no conscious control over this excessive clenching and grinding, particularly when it occurs during sleep.
The appliance used to treat TMJ disorder (and bruxism) is a night guard. This is similar to the mouth guards worn by athletes. The thin plastic framework is worn over the teeth at night to reduce the force placed on the teeth, gums, and jaws. The custom night guard is made with quality materials and the right thickness from the front to the back of the mouth, ensuring the proper distribution of protection.
The appliance used to treat TMJ disorder (and bruxism) is a night guard. This is similar to the mouth guards worn by athletes. The thin plastic framework is worn over the teeth at night to reduce the force placed on the teeth, gums, and jaws. The custom night guard is made with quality materials and the right thickness from the front to the back of the mouth, ensuring the proper distribution of protection.
Copyright © 2018 Classic Dental Clinic . All rights reserved